Newly Diagnosed With Type 2 Diabetes ... Or Type 3c Diabetes or LADA ... Who Knows!
I was surprised by my recent type 2 diabetes diagnosis because I didn't have prediabetes and my A1C shot up quickly.
Disclaimer: Please remember that this is not medical advice. Consult with your healthcare team for medical advice.
Over the years, I have checked my blood sugar many, many times while training school staff members and caregivers on how to help manage my child’s type 1 diabetes (T1DM), as well as during visits to pharma and medical device company headquarters to learn about new treatments. My friends with diabetes often joked that no matter how hard I tried, I just didn’t have diabetes.
In the past few years, I have dealt with painful and scary episodes of idiopathic pancreatitis. I have had pseudo cysts, have had drainage stents put in and taken out, had necrosis, and even had my gall bladder removed.
As recently as last summer, I had an A1c in the normal range.
So it surprised me that during routine bloodwork, my A1c came back at 7.6.
Wait. What?!
I got a message from the physician that I have type 2 diabetes (T2DM), to begin taking metformin, and to schedule appointments with a diabetes educator, dietitian, and endocrinologist.
Since I know a thing or two about diabetes (mostly type 1 diabetes), I almost instantly questioned how I could have developed type 2 diabetes rapidly, the onset of which is often slow. Plus, many people are diagnosed with prediabetes first as their blood sugars and A1c begin to creep up.
According to the American Diabetes Association (ADA), “Before people develop type 2 diabetes, they almost always have prediabetes, a health condition where your blood glucose is higher than normal but not as high as if you had diabetes.”
Type 3c Diabetes
I woudn’t say I was in denial, but I questioned the diagnosis because of the sudden onset. I first wondered if not having my gall bladder affects blood sugar. I headed to the NIH website and looked for information. (No, I didn’t use Dr. Google.) It then dawned on me that, duh, the frequent pancreatitis and necrosis might be to blame.
Two papers suggest this must be the case:
Bingo!
This took me down a rabbit hole.
This type of diabetes is called type 3c diabetes mellitus (T3cDM), pancreatogenic diabetes, post-acute pancreatitis diabetes (PAPD), and post-pancreatitis diabetes mellitus (PPDM). There is no simple test to confirm it definitively.
In the paper Diabetes mellitus as a consequence of acute severe pancreatitis: Unraveling the mystery, the authors state, “The diagnosis of PPDM should be suspected in all patients with a history of pancreatitis and fulfilling the diagnostic criteria for diabetes by the ADA. The diagnosis of PPDM is more of a diagnosis of exclusion, after excluding the more common stress hyperglycemia, type 1 and type 2 diabetes.”
Here is a flowchart from the same paper:
I conferred with my gastroenterologist and primary care physician, and both stated that it would be treated the same as type 2 diabetes and to follow up with endocrinology, which, of course, isn’t for three months(!).
LADA
My other almost immediate thought was that I might have latent autoimmune diabetes in adults (LADA), which is often misdiagnosed as type 2 diabetes because of the slow onset. This could be a possibility since I have a first-degree relative with type 1 diabetes. The authors of the paper Recognizing and Appropriately Treating Latent Autoimmune Diabetes in Adults explain:
Whereas type 1 diabetes often develops rapidly, LADA is not as rapid and presents like a slowly progressing form of type 1 diabetes. Because β-cell function is lost more gradually than in type 1 diabetes but more rapidly than in type 2 diabetes, patients may initially respond to noninsulin glucose-lowering agents. However, once β-cell function declines, their response to these agents will diminish.
Patients with LADA who are incorrectly diagnosed with type 2 diabetes often will be started down a path of various oral treatment options, potentially delaying effective treatment. Although, as noted, LADA patients may initially respond to oral medications, they often require insulin therapy within 5 years of diagnosis. Providers may spend several months titrating oral medications, suspecting nonadherence, and enforcing further lifestyle modifications when, in actuality, these patients are in need of insulin therapy. Medications that preserve β-cell function may be useful for LADA as well, given its relatively more rapid progression of β-cell loss compared to type 2 diabetes. Incorrect diagnosis can delay proper treatment, exposing patients to potential adverse effects from ineffective drugs, slowing progress toward normoglycemia, and ultimately increasing the risk of long-term complications.
Blood tests for islet cell autoantibodies (ICA), autoantibodies to glutamic acid decarboxylase (GAD), tyrosine phosphatase–related islet antigen 2 (IA-2), and insulin autoantibodies (IAA) can help identify LADA.
I talked my primary care physician into doing the antibody tests, but she was unable to order them. When I met with the diabetes educator, she asked the endocrinologist if they could go ahead and order it, but I was advised that we could discuss it during my appointment in July(!).
If I do have LADA, I would want the correct diagnosis and treatment so that we are not treating type 2 diabetes with oral medication and so that we can try to preserve β-cell function. Plus, both LADA and T3cDM may require insulin to manage blood sugar sooner rather than later, and I would want to start that as soon as needed to ease the burden on my body.
Diagnosis
My current diagnosis is type 2 diabetes. I am checking my fasting blood sugar each morning, and I have begun taking Metformin. But I am not ruling out a diagnosis of T3cDM or LADA and hope that the endocrinologist is open to investigating these possibilities. And if not, I will look for a second opinion. It’s frustrating that I cannot be seen for 3 months.
I am glad that I have a background in diabetes caregiving, education, and advocacy and that I don’t feel overwhelmed by the type 2 diabetes diagnosis. But for those who don’t have this background, I could see that it would be scary and daunting.
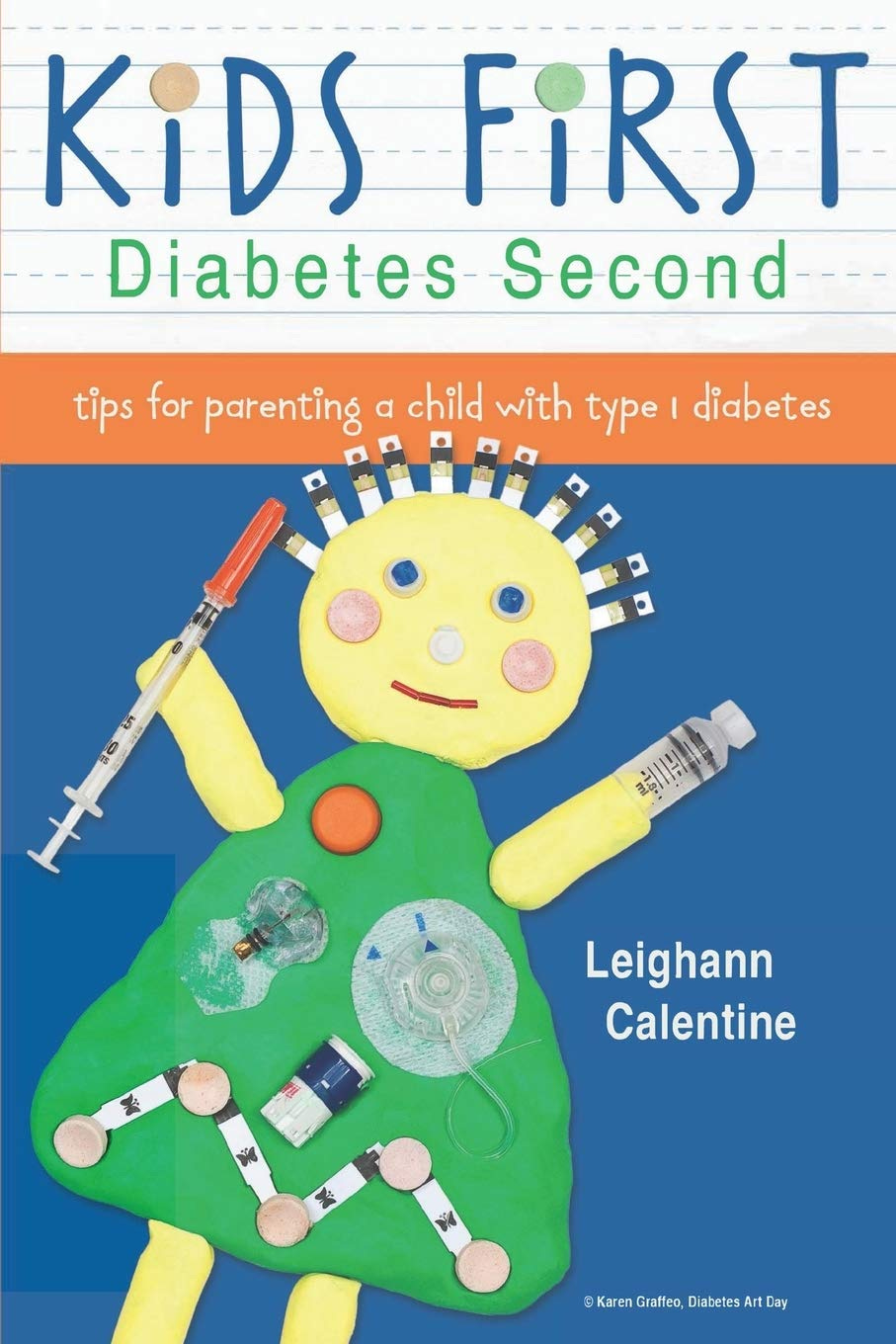
During my appointment with the diabetes educator, she half jokingly said, “You could probably write a book about this.” To which I replied, “Actually, I already did.”*
*I’m currently working on the second edition of my book Kids First, Diabetes Second. I’m also looking for a new agent and publisher for this edition, if you have recommendations.